×
Privacy Policy
INTRODUCTION
Welcome to the HIMSS Privacy Policy and notice.
HIMSS respects your privacy and is committed to protecting your personal data. This privacy notice will inform you as to how we look after your personal data when you personally interact with us or visit HIMSS websites (regardless of from where you visit) and tell you about your privacy rights and how the law protects you.
This privacy notice is provided in a layered format so you can click through to the specific areas set out below. Please also use the Glossary to understand the meaning of some of the terms used in this privacy notice.
1. IMPORTANT INFORMATION AND WHO WE ARE
2. THE DATA WE COLLECT ABOUT YOU
3. HOW IS YOUR PERSONAL DATA COLLECTED
4. HOW WE USE YOUR PERSONAL DATA
5. DISCLOSURES OF YOUR PERSONAL DATA
6. INTERNATIONAL TRANSFERS
7. DATA SECURITY
8. DATA RETENTION
9. YOUR LEGAL RIGHTS
10. GLOSSARY
1. IMPORTANT INFORMATION AND WHO WE ARE
PURPOSE OF THIS PRIVACY NOTICE
This privacy notice aims togive you information on how HIMSS collects and processes your personal data through your use of any HIMSS website, including any data you may provide through a HIMSS website when you sign up to our newsletter, purchase a product or service or take part in a competition.
HIMSS websites are not intended for children and we do not knowingly collect data relating to children.
It is important that you read this privacy notice together with any other privacy notice or fair processing notice we may provide on specific occasions when we are collecting or processing personal data about you so that you are fully aware of how and why we are using your data. This privacy notice supplements the other notices and is not intended to override them.
CONTROLLER
The Healthcare Information and Management Systems Society, a US not-for-profit corporation, is the controller and responsible for your personal data (collectively referred to as ”HIMSS” “we”, “us” or “our” in this privacy notice).
HIMSS includes the following different legal entities which may also act as controllers or processors of your personal data:
Healthcare Information and Management Systems Society
a US not-for-profit corporation organized in the State of Illinois
(includes the brand “Health 2.0”)
HIMSS Europe GmbH
UST ID.: DE 272998900 Handelsregistereintrag: HRB 152823 B
(includes the brand “HIMSS Analytics Europe”)
Citadel Events Ltd. trading as HIMSS UK, Company Number 05506954
HIMSS Media, LLC
a US limited liability company organized in the State of Maine
HIMSS Analytics, LLC
a US limited liability company organized in the State of Delaware
Healthbox Global Partners, LLC
a US limited liability company organized in the State of Delaware
Personal Connected Health Alliance, LLC
a US limited liability company organized in the State of Illinois
(includes the brand “Continua”)
This privacy notice is issued on behalf of the HIMSS group so when we mention ”HIMSS”, “we”, “us” or “our” in this privacy notice, we are referring to the relevant company in the HIMSS group responsible for processing your data. HIMSS is the controller and is ultimately responsible for your data.
We have appointed a data protection officer (DPO) who is responsible for overseeing questions in relation to this privacy notice. If you have any questions about this privacy notice, including any requests to exercise your legal rights, please contact the DPO using the details set out below.
CONTACT DETAILS
In the United States of America:
Healthcare Information and Management Systems Society
HIMSS Analytics, LLC
HIMSS Media, LLC
Healthbox Global Partners, LLC
Personal Connected Health Alliance, LLC
Attn: Data Protection Officer
4300 Wilson Boulevard, Suite 250
Arlington, VA 22203
USA
dpo-USA@himss.org
In the United Kingdom:
Citadel Events, Ltd. trading as HIMSS UK
HIMSS Europe GmbH
Attn: Data Protection Officer
Regent House
13-15 Albert St
Harrogate HG1 1JX
UNITED KINGDOM
dpo-UK@himss.org
In Germany:
HIMSS Europe GmbH
Attn: Data Protection Officer
Bertha-Benz-Straße 5
10557 Berlin
GERMANY
dpo-Germany@himss.org
You have the right to make a complaint at any time to the Information Commissioner’s Office (ICO), the UK supervisory authority for data protection issues (www.ico.org.uk) or the appropriate data protection supervisory authorities for the non-public sector in Germany Datenschutzaufsichtsbehörden für den nicht-öffentlichen Bereich. We would, however, appreciate the chance to deal with your concerns before you approach the ICO or the German data protection supervisory authorities so please contact us in the first instance.
CHANGES TO THE PRIVACY NOTICE AND YOUR DUTY TO INFORM US OF CHANGES
This version was last updated May 2018.
The data protection law in Europe will change on May 25, 2018. Although this privacy notice sets out most of your rights under the new laws, we may not yet be able to respond to some of your requests (for example, a request for the transfer of your personal data) until May 2018 as we are still working towards getting our systems ready for some of these changes.
It is important that the personal data we hold about you is accurate and current. Please keep us informed if your personal data changes during your relationship with us.
THIRD-PARTY LINKS
HIMSS websites may include links to third-party websites, plug-ins and applications. Clicking on those links or enabling those connections may allow third parties to collect or share data about you. We do not control these third-party websites and are not responsible for their privacy statements. After you leave a HIMSS website, we encourage you to read the privacy notice of every website you visit.
2. THE DATA WE COLLECT ABOUT YOU
Personal data, or personal information, means any information about an individual from which that person can be identified. It does not include data where the identity has been removed (anonymous data).
We may collect, use, store and transfer different kinds of personal data about you which we have grouped together follows:
Identity Data includes first name, maiden name, last name, username or similar identifier, marital status, title, date of birth and gender.
Contact Data includes billing address, delivery address, email address and telephone and fax numbers.
Financial Data includes bank account and payment card details.
Transaction Data includes details about payments to and from you and other details of products and services you have purchased from us.
Technical Data includes internet protocol (IP) address, your login data, browser type and version, time zone setting and location, browser plug-in types and versions, operating system and platform and other technology on the devices you use to access HIMSS websites.
Profile Data includes your username and password, purchases or orders made by you, your interests, preferences, feedback and survey responses.
Usage Data includes information about how you use our websites, products and services.
Marketing and Communications Data includes your preferences in receiving marketing from us and our third parties and your communication preferences.
We also collect, use and share Aggregated Data such as statistical or demographic data for any purpose. Aggregated Data may be derived from your personal data but is not considered personal data in law as this data does not directly or indirectly reveal your identity. For example, we may aggregate your Usage Data to calculate the percentage of users accessing a specific website feature. However, if we combine or connect Aggregated Data with your personal data so that it can directly or indirectly identify you, we treat the combined data as personal data which will be used in accordance with this privacy notice.
We do not collect any Special Categories of Personal Data about you (this includes details about your race or ethnicity, religious or philosophical beliefs, sex life, sexual orientation, political opinions, trade union membership, information about your health and genetic and biometric data). Nor do we collect any information about criminal convictions and offences.
IF YOU FAIL TO PROVIDE PERSONAL DATA
Where we need to collect personal data by law, or under the terms of a contract we have with you and you fail to provide that data when requested, we may not be able to perform the contract we have or are trying to enter into with you (for example, to provide you with goods or services). In this case, we may have to cancel a product or service you have with us but we will notify you if this is the case at the time.
3. HOW IS YOUR PERSONAL DATA COLLECTED?
We use different methods to collect data from and about you including through:
Direct interactions. You may give us your Identity, Contact and Financial Data by filling in forms or by corresponding with us by post, phone, email or otherwise. This includes personal data you provide when you:
apply for our products or services;
attend our events;
create an account on a HIMSS website;
subscribe to our service or publications;
download whitepapers or other content;
request marketing to be sent to you;
enter a competition, promotion or survey; or
give us some feedback.
Automated technologies or interactions. As you interact with a HIMSS website, we may automatically collect Technical Data about your equipment, browsing actions and patterns. We collect this personal data by using cookies, server logs and other similar technologies. We may also receive Technical Data about you if you visit other websites employing our cookies. Please see our cookie policy for further details.
Third parties or publicly available sources. We may receive personal data about you from various third parties and public sources as set out below:
Technical Data from the following parties:
(a) analytics providers based inside and outside the EU;
(b) advertising networks based inside and outside the EU; and
(c) search information providers based inside and outside the EU.
Contact, Financial and Transaction Data from providers of technical, payment and delivery services based inside and outside the EU.
Identity and Contact Data from data brokers or aggregators based inside and outside the EU.
Identity and Contact Data from publicly availably sources based inside and outside the EU.
4. HOW WE USE YOUR PERSONAL DATA
We will only use your personal data when the law allows us to. Most commonly, we will use your personal data in the following circumstances:
Where we need to perform the contract we are about to enter into or have entered into with you.
Where it is necessary for our legitimate interests (or those of a third party) and your interests and fundamental rights do not override those interests.
Where we need to comply with a legal or regulatory obligation.
Click here to find out more about the types of lawful basis that we will rely on to process your personal data.
Generally we do not rely on consent as a legal basis for processing your personal data other than in relation to sending third party direct marketing communications to you via email or text message. You have the right to withdraw consent to marketing at any time by contacting us.
PURPOSES FOR WHICH WE WILL USE YOUR PERSONAL DATA
We have set out below, in a table format, a description of all the ways we plan to use your personal data, and which of the legal bases we rely on to do so. We have also identified what our legitimate interests are where appropriate.
Note that we may process your personal data for more than one lawful ground depending on the specific purpose for which we are using your data. Please contact us if you need details about the specific legal ground we are relying on to process your personal data where more than one ground has been set out in the table below.
Purpose/Activity Type of data Lawful basis for processing including basis of legitimate interest
To register you as a new customer
(a) Identity
(b) Contact
Performance of a contract with you
To process and deliver your order including:
(a) Manage payments, fees and charges
(b) Collect and recover money owed to us
(a) Identity
(b) Contact
(c) Financial
(d) Transaction
(e) Marketing and Communications
(a) Performance of a contract with you
(b) Necessary for our legitimate interests (to recover debts due to us)
To manage our relationship with you which will include:
(a) Notifying you about changes to our terms or privacy policy
(b) Asking you to leave a review or take a survey
(a) Identity
(b) Contact
(c) Profile
(d) Marketing and Communications
(a) Performance of a contract with you
(b) Necessary to comply with a legal obligation
(c) Necessary for our legitimate interests (to keep our records updated and to study how customers use our products/services)
To enable you to partake in a prize draw, competition or complete a survey
(a) Identity
(b) Contact
(c) Profile
(d) Usage
(e) Marketing and Communications
(a) Performance of a contract with you
(b) Necessary for our legitimate interests (to study how customers use our products/services, to develop them and grow our business)
To administer and protect our business and HIMSS websites (including troubleshooting, data analysis, testing, system maintenance, support, reporting and hosting of data)
(a) Identity
(b) Contact
(c) Technical
(a) Necessary for our legitimate interests (for running our business, provision of administration and IT services, network security, to prevent fraud and in the context of a business reorganisation or group restructuring exercise)
(b) Necessary to comply with a legal obligation
To deliver relevant website content and advertisements to you and measure or understand the effectiveness of the advertising we serve to you
(a) Identity
(b) Contact
(c) Profile
(d) Usage
(e) Marketing and Communications
(f) Technical
Necessary for our legitimate interests (to study how customers use our products/services, to develop them, to grow our business and to inform our marketing strategy)
To use data analytics to improve HIMSS websites, products/services, marketing, customer relationships and experiences
(a) Technical
(b) Usage
Necessary for our legitimate interests (to define types of customers for our products and services, to keep HIMSS websites updated and relevant, to develop our business and to inform our marketing strategy)
To make suggestions and recommendations to you about goods or services that may be of interest to you
(a) Identity
(b) Contact
(c) Technical
(d) Usage
(e) Profile
Necessary for our legitimate interests (to develop our products/services and grow our business)
MARKETING
We strive to provide you with choices regarding certain personal data uses, particularly around marketing and advertising. We have established a subscription management centre where you can view and edit the number of emails you want to receive from us. You will also be given the option to unsubscribe to all communications on the same subscription centre which is located at: http://go.himss.org/subscription-management.html
PROMOTIONAL OFFERS FROM US
We may use your Identity, Contact, Technical, Usage and Profile Data to form a view on what we think you may want or need, or what may be of interest to you. This is how we decide which products, services and offers may be relevant for you (we call this marketing).
You will receive marketing communications from us if you have requested information from us or purchased goods or services from us or if you provided us with your details when you entered a competition or registered for a promotion and, in each case, you have not opted out of receiving that marketing.
THIRD-PARTY MARKETING
We will get your express opt-in consent before we share your personal data with any company outside the HIMSS group of companies for marketing purposes.
OPTING OUT
You can ask us or third parties to stop sending you marketing messages at any time by visiting the subscription management centre at http://go.himss.org/subscription-management.html and checking or unchecking relevant boxes to adjust your marketing preferences; by following the opt-out links on any marketing message sent to you; or by contacting us at any time.
Where you opt out of receiving these marketing messages, this will not apply to personal data provided to us as a result of a product/service purchase, warranty registration, product/service experience or other transactions.
COOKIES
You can set your browser to refuse all or some browser cookies, or to alert you when websites set or access cookies. If you disable or refuse cookies, please note that some parts of HIMSS websites may become inaccessible or not function properly. For more information about the cookies we use, please see our cookie policy.
CHANGE OF PURPOSE
We will only use your personal data for the purposes for which we collected it, unless we reasonably consider that we need to use it for another reason and that reason is compatible with the original purpose. If you wish to get an explanation as to how the processing for the new purpose is compatible with the original purpose, please contact us.
If we need to use your personal data for an unrelated purpose, we will notify you and we will explain the legal basis which allows us to do so.
Please note that we may process your personal data without your knowledge or consent, in compliance with the above rules, where this is required or permitted by law.
5. DISCLOSURES OF YOUR PERSONAL DATA
We may have to share your personal data with the parties set out below for the purposes set out in the table in paragraph 4 above.
You, and where appropriate, your family, your associates and your represenatives;
Members, sponsors and other clients of our business;
Credit reference agencies;
Anti-fraud services
Government, legal, regulatory or similar authorities, ombudsmen, and central and/or local government agencies, upon request or where required, including for the purposes of reporting any actual or suspected breach of applicable law or regulation;
Accountants, auditors, financial advisors, lawyers and other outside professional advisors to HIMSS, subject to binding contractual obligations of confidentiality;
Debt-collection agencies and tracing agencies;
Data aggregations services;
Accreditation bodies;
Third party Processors (such as payment service providers, shipping companies, etc.)
Any relevant party, claimant, complainant, enquirer, law enforcement agency or court, to the extent necessary for the establishment, exercise or defence of legal rights in accordance with applicable law;
Any relevant party for the purposes of prevention, investigation, detection or prosecution of criminal offences or the execution of criminal penalties, including safeguarding against and the prevention of threats to public security in accordance with applicable law;
Any relevant third party acquirer(s), in the event we sell or transfer all or any portion of our business or assets (including in the event of a reorganization, dissolution or liquidation);
The press and the media; and
Voluntary and charitable organizations.
HIMSS’ platforms, including social media platforms, may use third party plug-ins or content. If you opt to interact with such plug-ins or content, your Personal Data may be shared with the third party provider of the relevant platform. We encourage and recommend that you review that third party’s privacy policy before interacting with its plug-ins or content.
We require all third parties to respect the security of your personal data and to treat it in accordance with the law. We do not allow our third-party service providers to use your personal data for their own purposes and only permit them to process your personal data for specified purposes and in accordance with our instructions.
6. INTERNATIONAL TRANSFERS
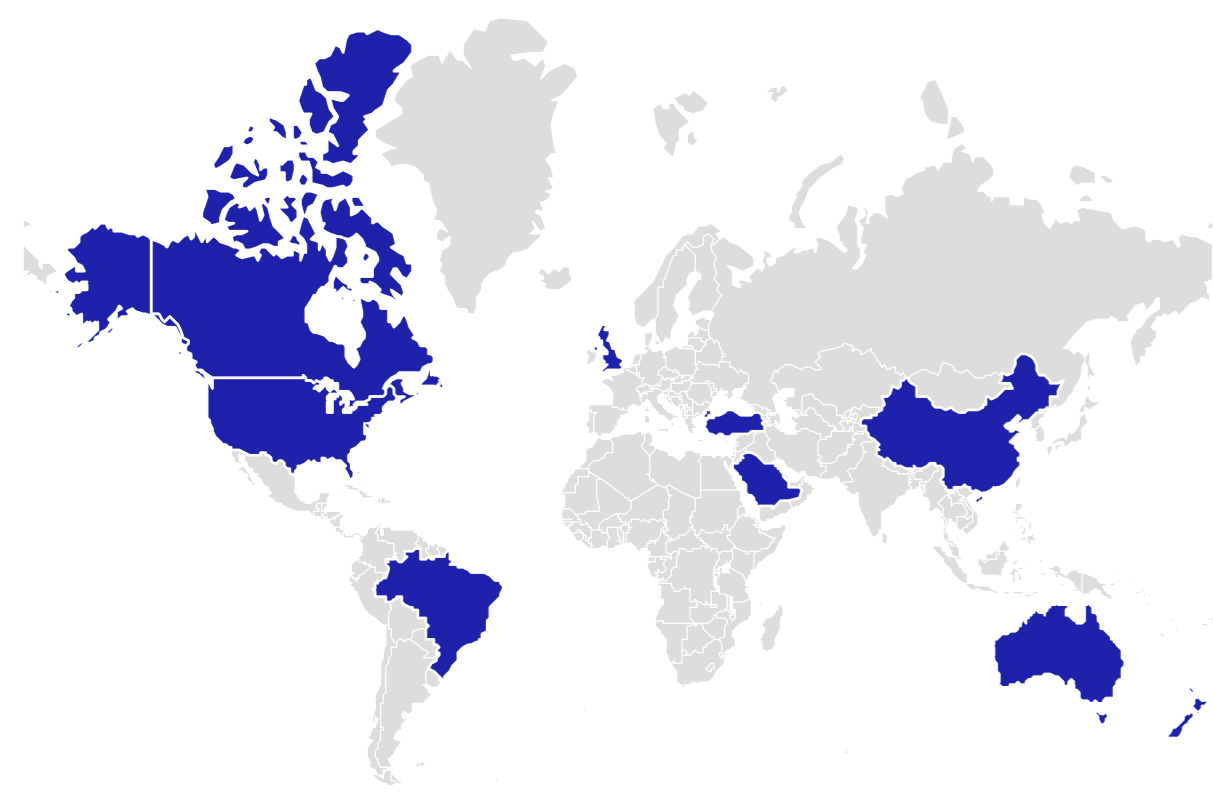
We share your personal data within the HIMSS Group. This will involve transferring your data outside the European Economic Area (EEA).
We ensure your personal data is protected by requiring all our group companies to follow the same rules when processing your personal data. These rules are called “binding corporate rules”.
Many of our external third parties are based outside the European Economic Area so their processing of your personal data will involve a transfer of data outside the EEA.
Whenever we transfer your personal data out of the EEA, we ensure a similar degree of protection is afforded to it by ensuring the following safeguard is implemented:
Where we use certain service providers, we may use specific contracts approved by the European Commission which give personal data the same protection it has in Europe.
Please contact us if you want further information on the specific mechanism used by us when transferring your personal data out of the EEA.
7. DATA SECURITY
We have put in place appropriate security measures to prevent your personal data from being accidentally lost, used or accessed in an unauthorised way, altered or disclosed. In addition, we limit access to your personal data to those employees, agents, contractors and other third parties who have a business need to know. They will only process your personal data on our instructions and they are subject to a duty of confidentiality.
We have put in place procedures to deal with any suspected personal data breach and will notify you and any applicable regulator of a breach where we are legally required to do so.
8. DATA RETENTION
HOW LONG WILL YOU USE MY PERSONAL DATA FOR?
We will only retain your personal data for as long as necessary to fulfil the purposes we collected it for, including for the purposes of satisfying any legal, accounting, or reporting requirements.
To determine the appropriate retention period for personal data, we consider the amount, nature, and sensitivity of the personal data, the potential risk of harm from unauthorised use or disclosure of your personal data, the purposes for which we process your personal data and whether we can achieve those purposes through other means, and the applicable legal requirements.
By law we have to keep basic information about our customers (including Contact, Identity, Financial and Transaction Data) for six years after they cease being customers for tax purposes.
In some circumstances you can ask us to delete your data: see request erasure below for further information.
In some circumstances we may anonymise your personal data (so that it can no longer be associated with you) for research or statistical purposes in which case we may use this information indefinitely without further notice to you.
9. YOUR LEGAL RIGHTS
Under certain circumstances, you have rights under data protection laws in relation to your personal data. Please click on the links below to find out more about these rights:
Request access to your personal data.
Request correction of your personal data.
Request erasure of your personal data.
Object to processing of your personal data.
Request restriction of processing your personal data.
Request transfer of your personal data.
Right to withdraw consent.
If you wish to exercise any of the rights set out above, please contact us.
NO FEE USUALLY REQUIRED
You will not have to pay a fee to access your personal data (or to exercise any of the other rights). However, we may charge a reasonable fee if your request is clearly unfounded, repetitive or excessive. Alternatively, we may refuse to comply with your request in these circumstances.
WHAT WE MAY NEED FROM YOU
We may need to request specific information from you to help us confirm your identity and ensure your right to access your personal data (or to exercise any of your other rights). This is a security measure to ensure that personal data is not disclosed to any person who has no right to receive it. We may also contact you to ask you for further information in relation to your request to speed up our response.
TIME LIMIT TO RESPOND
We try to respond to all legitimate requests within one month. Occasionally it may take us longer than a month if your request is particularly complex or you have made a number of requests. In this case, we will notify you and keep you updated.
10. GLOSSARY
LAWFUL BASIS
Legitimate Interest means the interest of our business in conducting and managing our business to enable us to give you the best service/product and the best and most secure experience. We make sure we consider and balance any potential impact on you (both positive and negative) and your rights before we process your personal data for our legitimate interests. We do not use your personal data for activities where our interests are overridden by the impact on you (unless we have your consent or are otherwise required or permitted to by law). You can obtain further information about how we assess our legitimate interests against any potential impact on you in respect of specific activities by contacting us.
Performance of Contract means processing your data where it is necessary for the performance of a contract to which you are a party or to take steps at your request before entering into such a contract.
Comply with a legal or regulatory obligation means processing your personal data where it is necessary for compliance with a legal or regulatory obligation that we are subject to.
THIRD PARTIES
INTERNAL THIRD PARTIES
Other companies in the HIMSS Group acting as joint controllers or processors and who are based in the United States, the United Kingdom and Germany provide IT and system administration services and undertake leadership reporting.
EXTERNAL THIRD PARTIES
Service providers acting as processors based the United States, the United Kingdom and Germany who provide IT and system administration services.
Professional advisers acting as processors or joint controllers including lawyers, bankers, auditors and insurers based the United States, the United Kingdom and Germany who provide consultancy, banking, legal, insurance and accounting services.
HM Revenue & Customs, regulators and other authorities acting as processors or joint controllers based in the United Kingdom who require reporting of processing activities in certain circumstances.
YOUR LEGAL RIGHTS
You have the right to:
Request access to your personal data (commonly known as a “data subject access request”). This enables you to receive a copy of the personal data we hold about you and to check that we are lawfully processing it.
Request correction of the personal data that we hold about you. This enables you to have any incomplete or inaccurate data we hold about you corrected, though we may need to verify the accuracy of the new data you provide to us.
Request erasure of your personal data. This enables you to ask us to delete or remove personal data where there is no good reason for us continuing to process it. You also have the right to ask us to delete or remove your personal data where you have successfully exercised your right to object to processing (see below), where we may have processed your information unlawfully or where we are required to erase your personal data to comply with local law. Note, however, that we may not always be able to comply with your request of erasure for specific legal reasons which will be notified to you, if applicable, at the time of your request.
Object to processing of your personal data where we are relying on a legitimate interest (or those of a third party) and there is something about your particular situation which makes you want to object to processing on this ground as you feel it impacts on your fundamental rights and freedoms. You also have the right to object where we are processing your personal data for direct marketing purposes. In some cases, we may demonstrate that we have compelling legitimate grounds to process your information which override your rights and freedoms.
Request restriction of processing of your personal data. This enables you to ask us to suspend the processing of your personal data in the following scenarios: (a) if you want us to establish the data’s accuracy; (b) where our use of the data is unlawful but you do not want us to erase it; (c) where you need us to hold the data even if we no longer require it as you need it to establish, exercise or defend legal claims; or (d) you have objected to our use of your data but we need to verify whether we have overriding legitimate grounds to use it.
Request the transfer of your personal data to you or to a third party. We will provide to you, or a third party you have chosen, your personal data in a structured, commonly used, machine-readable format. Note that this right only applies to automated information which you initially provided consent for us to use or where we used the information to perform a contract with you.
Withdraw consent at any time where we are relying on consent to process your personal data. However, this will not affect the lawfulness of any processing carried out before you withdraw your consent. If you withdraw your consent, we may not be able to provide certain products or services to you. We will advise you if this is the case at the time you withdraw your consent.